Impact
The impact we’re making together
Case Studies
Explore a collection of in-depth case studies that reveal how mental health training made the difference in so many different industries.
Testimonials
Delve into research studies that unveil the power of our training. Explore the data-driven proof of how Opening Minds makes a difference.

When Wellness Becomes a Performance: Eating Disorders, Language, and Shared Spaces
Understanding Eating Disorders
Eating disorders are widely misunderstood.
They are often framed as personal choices, lifestyle extremes, or issues of willpower and discipline. In reality, eating disorders are serious, clinically diagnosed mental illnesses shaped by a complex interaction of biological, psychological, and social factors.
No single comment, colleague, or leader causes an eating disorder. But environments matter. Repeated messages, shared norms, and everyday interactions can increase vulnerability – or reinforce recovery -especially for someone already at risk.
An eating disorder is a clinically diagnosed mental health condition characterized by persistent disturbances in eating behaviours, thoughts, and emotions related to food, weight, and body image. These disturbances significantly impair physical health, psychological well-being, and daily functioning.
Eating disorders are not lifestyle choices or phases. They are treatable mental illnesses influenced by biology (including genetics and brain chemistry), psychology (such as perfectionism, trauma, and coping styles), and social and environmental factors, including weight stigma and cultural norms.
Diagnosis is made by a qualified health professional using standardized criteria, most commonly the DSM-5-TR.
“No single person causes an eating disorder, but the environments we create can either increase risk or support recovery.”
Shared spaces, workplaces, homes, and communities, play a role in shaping what behaviours are normalized, praised, or tolerated. Language doesn’t just reflect culture; it helps build it.
The Spaces we Make
Words are powerful, they can create safety and support. Unfortunately, much of the language around eating and body image in our society can be stigmatizing or triggering.
Consider scenarios we may encounter in our workplaces.
Scenario 1: When food becomes a performance
Imagine a team, leaders and colleagues alike, where restrictive eating is openly discussed and admired.
Someone talks about cutting sugar, avoiding certain foods, or “being disciplined.” When they successfully restrict, they share it. When others eat differently, there are comments, sometimes framed as personal preference.
“I could never eat that.” “That’s so much sugar.”
No one intends harm.
And repetition matters.
Over time, the lunchroom changes. What was once a place for rest, connection, and refuelling becomes performative. People adjust what they bring. Foods are hidden. Conversation tightens. Some people stop eating in shared spaces altogether.
This isn’t about one person’s choices. It’s about what the group learns is acceptable, admirable, or risky.
Scenario 2: When wellness rewards control
Consider a hydration or wellness challenge.
It looks supportive. It encourages a healthy habit. Participation is optional. There’s tracking, visibility, and recognition for those who “win.”
But beneath that is a familiar structure:
- Monitoring consumption
- Public comparison
- Discipline as achievement
For someone already vulnerable, this can quietly reinforce a dangerous equation: control equals worth.
Again, no bad intent. But intent alone doesn’t shape impact.
“When health is measured through visibility and comparison, care quietly gives way to control.”
Restriction as a cultural signal
Across many settings, not just workplaces, restriction is often treated as a marker of responsibility or success.
You hear it in everyday language:
- “I’m being good today”
- “I earned this”
- “I was so bad this weekend”
You see it in:
- Praise for weight loss without context
- Food rules framed as “clean” or “healthy”
- Wellness narratives that equate discipline with virtue
These messages don’t affect everyone equally. For some, they reinforce shame, rigidity, and silence.
Language as a lever for psychological health and safety
Language is one of the most accessible ways to reduce harm.
This isn’t about silence or perfection. It’s about intentional choice, especially in environments shaped by power, belonging, and visibility.
A few growth-oriented shifts:
- Instead of: “You look great! Have you lost weight?”
Try: “It’s good to see you.” - Instead of: “I had a big family dinner. I was so bad with food this weekend”
Try: “I had a good weekend.” - Instead of: “I could never eat that”
Try: Making your choice without commentary.
These are guardrails, not rules. They support psychological health and safety by reducing unnecessary judgment, comparison, and pressure.
What we can do
We cannot and should not diagnose, monitor, or police each other’s eating behaviours. That’s not our role, and trying to do so can increase shame, secrecy, and harm.
What we can do is influence shared environments, social norms, and language in ways that reduce risk, support recovery, and foster psychological safety.
This looks like:
- Avoiding commentary on bodies and food choices
- Designing wellness initiatives that prioritize autonomy over tracking or comparison
- Valuing rest, connection, and mental health, not just discipline
- Remembering that our words land in histories and experiences beyond our own
Small, consistent signals in culture, what is praised, normalized, or joked about, matter far more than individual monitoring.
This isn’t about blame. It’s about shared responsibility, collective growth, and intentional culture.
Finding support
If you or someone you know is struggling with disordered eating or an eating disorder, help is available. In Canada, you can access support through:
- National Eating Disorder Information Centre (NEDIC): https://nedic.ca
- Canadian Mental Health Association (CMHA): https://cmha.ca
- Kids Help Phone (for youth and young adults): https://kidshelpphone.ca
Early support can make a difference. No one should face these challenges alone.
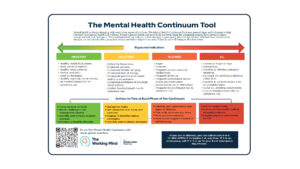
Learn more about training to help you build the skills and confidence to support someone who may be experiencing a decline in mental health with Mental Health First Aid, or how to spot the signs of shifts in mental health through the Mental Health Continuum with The Working Mind.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR)
- World Health Organization. International Classification of Diseases (ICD-11)
- National Eating Disorders Association (NEDA). Eating Disorders & Disordered Eating
- Canadian Mental Health Association (CMHA). Eating Disorders
- Academy for Eating Disorders (AED). Public Health & Prevention Frameworks
- National Institute for Health and Care Excellence (NICE). Eating Disorder Guidelines

The Duty to Inquire and Mental Health at Work: What Canadian Employers Need to Know
Supporting Mental Health in the workplace isn’t just good practice, in Canada, there are legal expectations tied to human rights and accommodation. One important concept employers should understand is the duty to inquire.
What Is the Duty to Inquire?
In Canadian workplace law, the duty to inquire is part of an employer’s broader duty to accommodate employees with disabilities, including Mental Health conditions. It means that when an employer knows or reasonably ought to know an employee might be experiencing a Mental Health issue that affects their work, the employer must initiate a respectful conversation about whether accommodation is needed before taking any negative action. (Canadian Human Rights Commission, Developing a Workplace Accommodation Policy)
For example, a long-standing high performer who suddenly starts struggling with deadlines or a team member showing consistent absenteeism or behaviour changes may trigger the employer’s duty to inquire and explore support options. (HRD Canada, Accommodating Mental Disabilities: Key Considerations for Employers)
Importantly, this does not mean employers diagnose mental illnesses or collect sensitive health details. Instead, they should ask open, supportive questions and focus on understanding functional needs; what assistance or changes might help the person do their job effectively. (Perlaw.ca, Navigating Mental Health Concerns in the Workplace)
Why This Matters in Canada
Under the Ontario Human Rights Code and similar human rights laws across Canada, Mental Health conditions, including anxiety, depression, PTSD, and others, are protected as disabilities. Employers are required to accommodate these to the point of undue hardship. (Ontario Government, Mental Health in the Workplace)
The Ontario Human Rights Commission clearly outlines that when an employer notices signs that someone may be experiencing significant difficulty at work due to a disability, the employer must inquire and offer assistance or accommodation options. This obligation applies even if the employee has not directly asked for help. (OHRC, Preventing Discrimination Based on Mental Health and Addiction Disabilities)
Failure to inquire before taking punitive action, such as termination or disciplinary measures, may be considered discriminatory under human rights law. Legal cases and tribunal decisions have repeatedly reinforced this procedural obligation. (OHRC, Policy on the Duty to Accommodate)
How Employers Should Respond
When an employer identifies potential concerns, they should:
- Ask open, respectful questions focused on how the employee is doing and whether there are barriers affecting their performance.
- Respect privacy and dignity by not demanding medical diagnoses or invasive details, only what is needed to understand accommodation needs.
- Explore accommodation options together with the employee, discussing reasonable workplace adjustments.
- Document discussions and check in regularly.
These practices are not just legal “tick-boxes.” They reflect best practices for supportive workplaces that respect rights and promote psychological safety.
Beyond Legal Compliance: Building a Mentally Healthy Workplace
Understanding the duty to inquire is important, but it is only one piece of a psychologically healthy and safe culture. Many employers struggle with knowing what to say and do when mental health concerns come up. Training and mental health literacy help organizations respond with confidence and care.
How can you equip your team to support this process?
The Working Mind (TWM) is Canada’s evidence-based mental health training program that helps workplaces:
- Recognize early signs of mental health challenges
- Reduce stigma and increase confidence in having supportive conversations
- Understand how to respond and connect people with resources
- Build psychologically healthy and safe spaces
Equipping managers and employees with the right skills makes it easier to fulfill the duty to inquire with empathy and confidence, creating workplaces where people are supported before issues escalate.
Learn more about The Working Mind and how it can support your organization today.
—Disclaimer: This article is for educational purposes only and does not constitute legal advice—

The Power of Conversation: Reflections from a Mental Health First Aider
Today, people across the country are talking about Mental Health. Whether they are reaching out to a friend or becoming in tune with their own Mental Health baseline, days like this are a reminder that support is out there and that even small words can make a difference.
Powerful moments
For me, these moments are powerful because I’ve seen first-hand what it’s like when someone feels truly heard. I’m a Mental Health First Aider, and part of my training was learning how to listen, ask the right questions, and connect people with the support they need. Training doesn’t give me all the answers, but it gives me the confidence to show up, to ask, and to be present.
Awareness is the first step
Awareness is the first step. It opens the door. But it’s the skills, the practice, and the courage to speak and listen is what keeps that door open. That’s what Mental Health First Aid teaches. It’s why I feel capable of engaging in conversations that might feel scary or awkward and why I know the small words I choose matter.
It’s as simple as asking, “Are you okay?”
Sometimes it’s as simple as asking, “Are you okay?” or noticing when someone seems quieter than usual. Other times, it’s about gently exploring what or who someone leans on when things feel heavy. The training gives me the tools, but moments like today remind me why they matter. They remind me that words have power and that conversations can be the start of something real.
Raising awareness about Mental Health
I’m grateful for initiatives like Bell Let’s Talk, initiatives that create space for people to have these important conversations and help push Mental Health forward in our communities. Raising awareness about Mental Health should span more than just a single day. Safe language, support, and unlearning should become vital parts of our daily routines. Today may spark the conversation, but the real impact happens when we continue to listen, act, and show up for each other. That’s what builds understanding, reduces stigma, and makes mental health a shared responsibility, one conversation at a time.
Talk to us
Interested in mental health training for your organization? Let us know
Testimonials
Hear from individuals whose lives and workplaces have been transformed by our mental health training. Opening Minds makes a real difference.
Evidence
When Wellness Becomes a Performance: Eating Disorders, Language, and Shared Spaces
Evidence
The Duty to Inquire and Mental Health at Work: What Canadian Employers Need to Know
Evidence